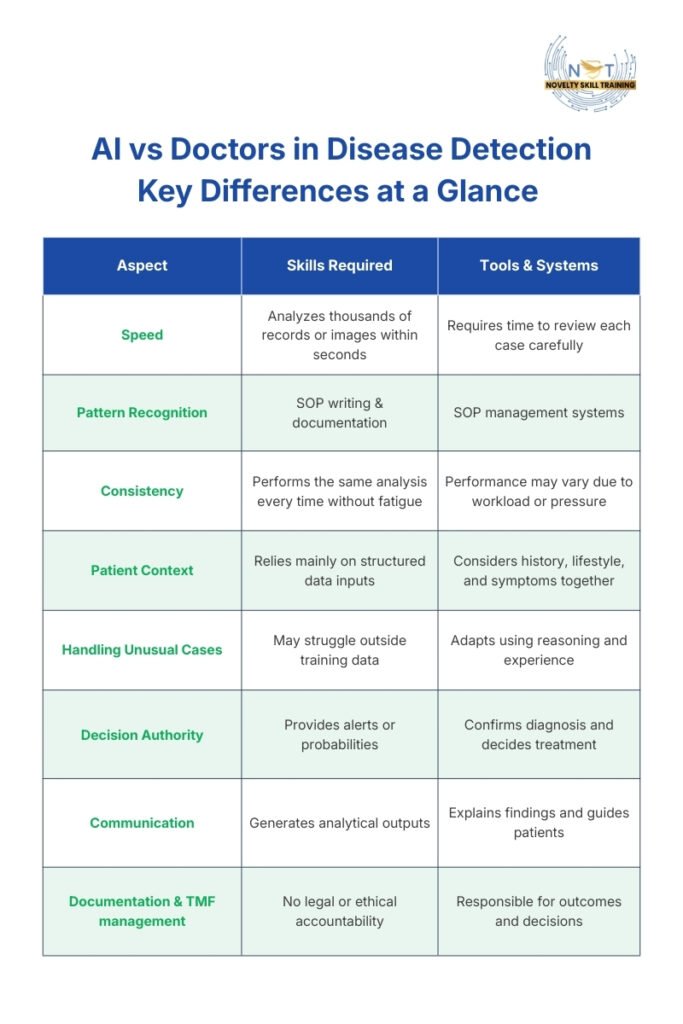
AI can detect certain diseases faster than humans by analyzing large amounts of medical data and identifying small patterns in scans, lab results, and patient records. However, doctors remain essential because diagnosis requires clinical judgment, patient context, and responsibility for treatment decisions.
Artificial intelligence is increasingly being used to read medical scans, analyze laboratory results, and identify early signs of disease. In some cases, AI systems have matched or even exceeded human-level accuracy in specific detection tasks. Research shows that artificial intelligence can perform on par with clinicians in diagnostic tasks, highlighting the technology’s growing accuracy and reliability in disease detection. This rapid growth of AI in disease detection has raised an important question in modern healthcare: if machines can analyze medical data faster and more consistently than humans, can AI actually detect diseases better than doctors?
The rise of artificial intelligence in healthcare has accelerated investment in diagnostic support systems across hospitals and research environments.
The answer depends on what disease detection actually involves. Detecting a disease is not only about finding abnormalities in images or numbers. It also requires understanding symptoms, medical history, patient risk factors, and deciding what those findings mean in real clinical situations. While AI is very strong at analyzing large amounts of data, medical decisions still depend on human judgment and responsibility.
To understand where artificial intelligence truly helps, it is important to separate capability from expectation. Many discussions framed as is AI better than doctors oversimplify the complexity of clinical care. This blog explains how AI detects diseases, where it performs better than humans, where doctors remain essential, and why modern healthcare increasingly relies on collaboration between both.
“AI will not replace doctors, but doctors who use AI will replace those who don’t.”— Eric Topol, Cardiologist & Digital Medicine Researcher In essence: Topol emphasizes that AI is a powerful support tool that enhances diagnostic accuracy, efficiency, and decision-making. Physicians who adopt AI can detect diseases earlier, analyze data more effectively, and improve patient outcomes — giving them a clear advantage in modern healthcare. |
What Is AI Disease Detection in Healthcare?
AI disease detection in healthcare refers to the use of advanced AI diagnostic tools to analyze medical data and identify possible signs of illness. These systems examine information such as medical images, blood test results, electronic health records, and vital signs to detect patterns linked to specific diseases.
The aim of AI in disease detection is to support faster and more reliable identification of medical problems.
AI systems in healthcare are trained on large, clinically validated datasets where diagnoses have been confirmed by medical professionals. These datasets, such as imaging scans, lab reports, and electronic health records, undergo quality review before being used for model development. By learning patterns from thousands of documented cases, AI can assist clinicians by highlighting suspicious areas on scans, flagging abnormal lab values, or identifying risk trends that may require further evaluation. In imaging departments, radiology AI tools are commonly used to help detect subtle abnormalities that may be difficult to identify consistently. These technologies operate within regulated healthcare frameworks and are designed to support, not replace, clinical judgment.
In real healthcare settings, many of these AI diagnostic solutions are integrated into broader clinical decision support AI platforms. These systems provide alerts or probability scores directly within hospital record systems, allowing healthcare professionals to interpret results, confirm findings, and decide the next steps in diagnosis or treatment.
The purpose of AI disease detection is therefore not to replace medical expertise, but to improve speed, reduce missed findings, and help clinicians identify potential problems earlier.
When Does AI in Disease Detection Perform Better Than Doctors?
Artificial intelligence performs better than humans in disease detection when tasks involve large volumes of data, repeated analysis, or very small changes that must be compared across many similar cases. These situations rely more on pattern recognition and consistency than on interpretation or decision-making. AI systems do not get tired, distracted, or influenced by workload, which allows them to maintain the same level of analysis across thousands of cases.
These strengths explain why AI in disease detection is particularly effective in technical and repetitive environments.
AI systems do not get tired, distracted, or influenced by workload, which allows them to maintain the same level of analysis across thousands of cases. Debates around AI vs doctors’ diagnosis often miss that both bring different strengths.
This does not mean AI replaces medical expertise. It means AI improves detection in specific technical tasks where scale and consistency matter most.
1.Medical Imaging and Radiology AI Tools
Medical imaging is currently the most established and widely used area for AI disease detection. Radiologists often review hundreds of scans daily, including X-rays, CT scans, MRIs, and mammograms. Even experienced specialists can miss very small abnormalities when reviewing large volumes of images under time pressure.
In modern hospitals, many of these systems are categorized as radiology AI tools, designed to assist radiologists by highlighting suspicious areas, prioritizing high-risk scans, and reducing reporting delays. These AI diagnostic tools function as a second reader, improving workflow efficiency while maintaining physician oversight.
Studies frequently measure AI disease detection accuracy by comparing results against specialist interpretations.
AI systems are trained using large, labeled image datasets where diseases have already been confirmed. During training, advances in machine learning in medical diagnosis allow systems to refine recognition of tumors, lung nodules, fractures, internal bleeding, or retinal damage.
For beginners, the important point is that AI does not “understand” the disease. It detects visual similarity and statistical patterns. This makes it especially effective at identifying subtle changes that are difficult to notice consistently.
In practice, AI acts as a second reader. The radiologist still confirms whether the highlighted area is clinically meaningful, but AI reduces the chance that early warning signs are overlooked.
2.Early Risk Detection and Prediction
Many diseases develop gradually before symptoms become visible. Humans are good at identifying clear problems, but less effective at recognizing slow changes across large datasets over time. AI performs well here because it can analyze historical trends rather than single test results.
A major benefit is AI early disease detection, enabling intervention before patients become critically
AI systems examine electronic health records, lab values, medication history, and vital signs to identify patterns linked to future complications. Many hospitals implement these systems under broader clinical decision support AI platforms, where risk alerts are integrated directly into electronic health record systems. This allows clinicians to receive real-time notifications without disrupting existing workflows.
For beginners, this is an important distinction. AI is not only used to detect existing disease. It is also used to estimate probability. The system calculates risk scores that help doctors decide whether closer monitoring or preventive treatment is necessary.
This shift allows healthcare to move from reacting to illness toward preventing deterioration earlier, especially in conditions such as sepsis, heart failure, or diabetic complications.
In simple terms, AI helps detect risk earlier by identifying gradual changes that are difficult to notice through individual tests alone.
3.Large-Scale Screening Programs
Screening programs aim to identify diseases in large populations, often before symptoms appear. Examples include breast cancer screening, diabetic eye disease screening, or lung imaging programs. These programs generate massive numbers of normal cases, with only a small percentage showing abnormalities.
Even when automation increases, AI medical diagnosis still requires physician validation to confirm real clinical relevance.
Human specialists reviewing every case manually can become overwhelmed, which increases delays and workload pressure. AI improves efficiency by automatically sorting cases based on risk. Normal scans can be cleared faster, while suspicious cases are prioritized for specialist review.
For beginners, the key idea is triage. AI helps decide which cases need attention first. It does not replace diagnosis. This approach allows healthcare systems to handle larger populations without reducing quality of care.
In simple terms, AI improves screening by helping doctors focus first on cases that are most likely to need medical attention.
4.Pathology and Laboratory Analysis
Pathology involves examining tissue samples or cells under a microscope to identify disease. This work requires extreme attention to detail because abnormalities may exist at a microscopic level. Small variations in cell structure or distribution can indicate serious conditions.
AI systems assist by scanning entire digital pathology slides and identifying regions that differ from known healthy patterns. They can count cells, measure structures, and detect irregularities consistently across very large samples. In laboratory settings, AI can also analyze relationships between multiple test results that may indicate early disease signals.
For beginners, the important point is consistency. Humans may vary in interpretation depending on workload or experience level, while AI applies the same analytical criteria every time. This makes AI useful as an additional verification layer rather than a replacement for specialist judgment.
In simple terms, AI improves pathology analysis by applying consistent review across large samples where small details matter.
5.Dermatology and Visual Assessment
Skin conditions are often evaluated visually, which makes dermatology suitable for AI-assisted detection. AI models trained on large image datasets can recognize patterns associated with suspicious moles, inflammatory conditions, or early signs of skin cancer.
This is particularly useful in primary care settings or remote consultations where dermatology specialists are not immediately available. AI can help identify which cases should be referred for further examination.
Beginners should understand that AI performs best in controlled image-based assessments. Factors such as lighting, image quality, and skin variation can affect accuracy, which is why final evaluation still requires clinical confirmation.
In simple terms, AI helps identify which skin conditions require faster specialist evaluation.
6.Continuous Patient Monitoring
In hospital and intensive care environments, patient data is generated continuously through monitoring devices. Heart rate, oxygen levels, blood pressure, and respiratory patterns change every second. Humans cannot continuously analyze these data streams in real time.
AI systems monitor these signals continuously and detect small deviations that may indicate deterioration. For example, subtle changes in multiple vital signs together may signal infection or organ stress before obvious symptoms appear.
For beginners, this demonstrates one of AI’s strongest advantages: constant observation. AI can identify patterns across time that are difficult for humans to track manually, allowing earlier medical intervention and improved patient safety.
In simple terms, AI improves monitoring by continuously tracking patient data and detecting early signs of deterioration.
Where Are Doctors Better Than AI at Detecting Diseases?
Doctors perform better than artificial intelligence in situations that require interpretation, contextual understanding, decision-making under uncertainty, and responsibility for patient outcomes. Disease detection is not only about identifying abnormalities in data or images. It also involves understanding how findings relate to a person’s symptoms, history, and overall health condition.
AI systems identify patterns based on training data, while doctors evaluate how those findings apply to the patient’s overall condition and treatment decisions.
1.Understanding the Patient Context
Doctors evaluate more than test results or scan findings. They consider medical history, lifestyle, family risk factors, ongoing medications, mental health, and current symptoms before reaching conclusions. Two patients with similar scan results may require completely different medical decisions depending on age, underlying conditions, or risk profile.
AI systems typically rely on structured inputs and predefined variables. They may not fully capture non-measurable factors such as symptom progression, patient behavior, or social and environmental influences. Physicians combine measurable data with clinical experience to determine whether a finding is significant or incidental.
For beginners, the important point is that AI highlights possible abnormalities, while doctors determine whether those findings are clinically meaningful.
2.Handling Complex and Unusual Cases
Real-world healthcare often involves patients with multiple conditions occurring at the same time. Symptoms may overlap, and test results may not follow typical patterns. AI models perform best when cases resemble the data they were trained on. When situations fall outside those patterns, accuracy can decrease.
Doctors, on the other hand, can reconsider assumptions, order additional investigations, and adjust their reasoning as new information becomes available. Clinical training allows physicians to handle ambiguity and adapt to unexpected findings.
Beginners should understand that medicine frequently deals with uncertainty, and flexibility in reasoning is something AI currently cannot replicate reliably.
3.Clinical Judgment and Decision-Making
AI systems usually provide probabilities, alerts, or risk scores rather than definitive answers. Turning those outputs into medical action requires judgment. Doctors must evaluate whether further testing is necessary, whether treatment risks outweigh benefits, and how decisions align with patient preferences and overall health goals.
Medical decisions often involve trade-offs. A test may detect disease earlier but also expose patients to unnecessary procedures or anxiety. Physicians weigh these factors before making recommendations.
For beginners, the key point is that detection alone is not diagnosis. Decision-making requires responsibility and accountability that remain in human roles.
4.Communication and Patient Interaction
Disease detection is not only a technical process. Patients need explanations, reassurance, and guidance after abnormal findings are identified. Doctors explain uncertainty, discuss possible outcomes, and help patients understand treatment options.
AI systems can generate analytical outputs but cannot respond to emotional concerns, answer follow-up questions meaningfully, or adapt communication based on individual patient needs. Effective communication also influences whether patients follow treatment recommendations, which directly affects outcomes.
5.Ethical and Legal Responsibility
Healthcare decisions carry ethical and legal consequences. Doctors are responsible for ensuring patient safety, maintaining confidentiality, and following medical standards and regulations. They must justify their decisions and remain accountable for outcomes.
AI systems do not hold responsibility for medical decisions. They function as tools within clinical workflows. Human oversight is required to ensure that AI recommendations are appropriate, unbiased, and applied safely.
For beginners, this explains why AI cannot independently diagnose or treat patients even if its technical accuracy improves.
AI and ML in Healthcare Training Course
Master artificial intelligence and machine learning to transform patient care, clinical research, and medical diagnostics. Learn how healthcare teams deploy predictive models, automate medical coding, and optimize workflows in modern clinical environments.
Duration: 6 Months
Skills you’ll gain:
- Healthcare Data Handling & Preparation
- Machine Learning Foundations
- Predictive Analytics in Clinical Settings
- AI for Diagnostics & Risk Stratification
- Model Evaluation & Validation
- Healthcare Data Visualization
- Responsible & Ethical AI Use
Other Courses
- Artificial Intelligence and Machine Learning Training
What Is the Future of AI in Disease Detection and Healthcare?
The future of AI in disease detection is centered on assistance and integration rather than replacement. Hospitals and healthcare systems are gradually incorporating AI tools into existing workflows to improve speed, reduce workload, and support earlier detection of medical problems. The goal is to help clinicians make better decisions by providing faster and more consistent analysis of medical data.
The expansion of AI in disease detection will continue to push healthcare toward earlier intervention and better prioritization.
One major change expected in the coming years is earlier detection through continuous data analysis. AI systems are becoming better at identifying small changes in imaging, laboratory trends, and patient monitoring data patterns that research shows can support earlier disease detection and improved clinical outcomes even before symptoms become severe. Earlier identification allows doctors to intervene sooner, helping reduce complications and improve treatment outcomes.
AI is also expected to handle more repetitive analytical tasks. AI can review large numbers of normal scans, monitoring routine patient data, or identifying low-risk cases can be partially automated. This allows healthcare professionals to spend more time on complex cases, patient communication, and decision-making where human expertise is most valuable, as research shows that AI can combine imaging and clinical data to improve diagnostic accuracy
Another important development is improving integration between different sources of medical information. Instead of analyzing images or lab results separately, In the future, AI systems combine multiple data types to provide a more complete clinical picture. For example, imaging findings, laboratory values, and patient history may be analyzed together to support earlier risk identification.
For beginners, it is important to understand that AI adoption in healthcare happens gradually. Medical systems require validation, regulation, and continuous human oversight before new technologies become routine, as emphasized in Who guidance and ethical and responsible use of AI in healthcare. Doctors will continue to guide how AI tools are used, ensuring that technology supports safe and meaningful patient care rather than replacing clinical responsibility.
Real Life ExampleAt Moorfields Eye Hospital NHS Foundation Trust, clinicians collaborated with Google DeepMind to develop an AI system that detects over 50 eye diseases from OCT retinal scans. Published in Nature Medicine (2018), the study showed the system performed at a level comparable to expert specialists in recommending urgent referrals. Designed to prioritize high-risk patients, the tool supports earlier detection and faster intervention, demonstrating how AI strengthens clinical workflows rather than replacing doctors. |
How Is the UAE Government Driving AI Adoption in Healthcare?
Artificial intelligence adoption in healthcare in the UAE is not happening only at the hospital level. It is being driven by national strategy, government policy, and long-term investment in digital health infrastructure. The UAE government has positioned artificial intelligence as a core part of its future healthcare and economic development plans, which is why AI integration is progressing faster compared to many other regions.
Investment in AI healthcare technology UAE is expanding rapidly across public systems.
The growth of AI in healthcare UAE reflects long-term digital transformation goals. As adoption expands, demand for expertise in AI medical diagnosis UAE is also increasing across hospitals and technology providers.
One of the main drivers is the UAE National Strategy for Artificial Intelligence 2031, which aims to establish the country as a global leader in AI and integrate intelligent technologies across priority sectors, including healthcare. The strategy focuses on building AI infrastructure, developing talent, and using data-driven technologies to improve government services and quality of life.
In healthcare specifically, this means increasing the use of predictive analytics, integrated data platforms, and AI-supported decision systems that help clinicians manage large volumes of medical information more efficiently.
At the operational level, UAE health authorities have already introduced AI-enabled initiatives to improve healthcare delivery. The Ministry of Health and Prevention has implemented AI-based smart healthcare operation centers designed to reduce emergency department waiting times and improve hospital resource management through data analysis. These systems demonstrate that AI is being used not only for disease detection but also for improving healthcare operations and patient flow.
Dubai has also introduced regulatory frameworks to guide safe AI adoption in healthcare. The Dubai Health Authority’s Artificial Intelligence Policy defines requirements around patient safety, transparency, privacy, and human oversight, ensuring that AI systems support doctors rather than operate independently. This regulatory approach allows innovation while maintaining clinical accountability.
In addition, government-backed initiatives such as Smart Dubai’s AI Lab have explored predictive AI applications capable of forecasting patient conditions and supporting earlier medical intervention. At a broader level, national programs are also investing in data platforms, genomics initiatives, and integrated health records to enable AI-driven preventive healthcare and precision medicine approaches.
For beginners and professionals in the UAE, this shift means that understanding how AI works in healthcare is becoming a practical career advantage rather than a future specialization. As healthcare organizations continue to integrate intelligent systems into clinical workflows, demand is growing for professionals who can work at the intersection of healthcare knowledge and AI-driven technology.
Who Should Learn AI and ML for Healthcare Applications?
As artificial intelligence becomes more common in healthcare environments, professionals who understand both medical workflows and AI systems are becoming increasingly valuable. Hospitals, healthcare technology companies, and research organizations are adopting AI tools to improve disease detection, patient monitoring, and operational efficiency. This creates a growing need for individuals who can work at the intersection of healthcare and data-driven technology.
Healthcare professionals benefit from understanding how AI systems analyze medical data, what their limitations are, and how to interpret outputs responsibly. Similarly, data professionals and engineers entering healthcare need domain knowledge to build models that align with real clinical requirements rather than purely technical objectives.
Learning AI and machine learning in a healthcare context helps individuals understand how medical data is prepared, how predictive models are evaluated, and how AI systems are applied safely in clinical environments. This knowledge is increasingly relevant for roles in healthcare analytics, clinical AI development, medical research, and healthcare technology implementation.
The AI and ML in Healthcare Training Program by Novelty Skills Training (NST-Dubai) is designed to introduce these concepts in a structured and practical way. The program focuses on real healthcare use cases, including disease prediction, medical data analysis, and responsible AI implementation, helping learners understand how intelligent systems support clinical decision-making rather than replace it.
Skills covered in this course includes healthcare data preparation, machine learning fundamentals, predictive analytics in clinical settings, AI-based risk analysis, model evaluation, healthcare data visualization, and ethical AI practices.
For beginners and professionals looking to transition into healthcare AI roles, structured training like this helps bridge the gap between theoretical AI knowledge and real-world healthcare applications.
Conclusion
Artificial intelligence is changing how diseases are detected, and this shift is also changing the skills required in modern healthcare. AI is already helping analyze medical images, identify risk patterns, and monitor patient data more efficiently. As healthcare systems continue to adopt these technologies, professionals who understand how AI supports clinical decision-making are becoming increasingly valuable.
At the same time, disease detection remains a human-led process. Doctors interpret findings, make decisions under uncertainty, and take responsibility for patient outcomes. This means the future of healthcare is not about replacing medical roles, but about expanding them. Healthcare professionals, data specialists, and technology professionals who can work alongside AI systems will be better positioned as healthcare becomes more data-driven.
In the UAE, government-led digital health initiatives and AI adoption are accelerating this transition. Hospitals and healthcare organizations are increasingly looking for individuals who understand both healthcare workflows and intelligent technologies. For beginners and professionals entering this field, developing skills in AI and machine learning within a healthcare context opens pathways into emerging roles across healthcare analytics, clinical AI, health technology, and medical research.
The future of disease detection will not be defined by AI or doctors working independently, but by how effectively both work together. Professionals who understand this collaboration and develop skills at the intersection of healthcare and artificial intelligence will be better positioned as the next phase of healthcare innovation continues to evolve.
Frequently Asked Questions (FAQs)
1. How accurate is AI in detecting diseases compared to doctors?
AI can reach high accuracy in specific tasks such as medical imaging or pattern recognition when trained on large datasets. However, accuracy depends on data quality and clinical context. Doctors validate AI findings and ensure that results match the patient’s overall condition before making medical decisions.
2. Does AI reduce diagnostic errors in healthcare?
AI can help reduce certain types of errors by acting as an additional review layer, especially in repetitive tasks like scan analysis or screening programs. It helps highlight abnormalities that may need attention, but final diagnosis still depends on medical evaluation.
3. Can AI detect diseases before symptoms appear?
In some cases, yes. AI systems can identify risk patterns in medical records, lab trends, or monitoring data that may indicate future complications. These predictions help doctors intervene earlier, but they are based on probability rather than certainty.
4. What types of medical data does AI use for disease detection?
AI systems commonly analyze medical images, laboratory results, electronic health records, vital signs, and sometimes genetic data. The system compares new data with previously learned patterns to identify possible abnormalities or risks.
5. Is AI used independently in hospitals today?
No. AI tools are used as decision-support systems. They assist healthcare professionals by providing alerts or analysis, but doctors review and confirm all findings before diagnosis or treatment decisions are made.
6. What are the limitations of AI in disease detection?
AI may struggle with rare diseases, unusual cases, or situations that differ from its training data. It also cannot understand patient emotions, lifestyle factors, or complex clinical judgment, which are essential parts of medical decision-making.
7. Do healthcare professionals need technical knowledge to work with AI tools?
Basic understanding is becoming increasingly useful. Healthcare professionals do not need to become programmers, but understanding how AI systems generate outputs helps in interpreting results safely and using them effectively in clinical workflows.
8. How is the UAE using AI in healthcare today?
The UAE is integrating AI through national initiatives such as the UAE National Strategy for Artificial Intelligence 2031. AI is being used to improve hospital operations, support diagnostic workflows, enhance patient monitoring, and enable data-driven healthcare planning.
9. Are AI-based healthcare systems regulated in Dubai and the UAE?
Yes. Authorities such as the Dubai Health Authority and the Ministry of Health and Prevention have introduced policies that require human oversight, patient data protection, and safety validation before AI systems are used in clinical environments.
10. Are there career opportunities in AI healthcare in the UAE?
Yes. As hospitals and healthcare technology companies adopt AI solutions, demand is increasing for professionals who understand healthcare data, machine learning applications, and AI-supported decision systems. Roles are emerging in healthcare analytics, clinical AI implementation, and health technology development.